I was in such a flare last week, I completely forgot it was Valentine’s Day when my newsletter went out.
When my brain registered it, I hurried onto Substack. Only to realize that the scheduled post went out two hours earlier.
I was a mess last week. This week, too.
I used to push myself, even when I was in so much pain I couldn’t move. I’d demand that my brain pick up the slack, even though it struggles, often, without prejudice. Especially when I’m in a mast cell flare.
I still push myself, at times. But it’s different. I have a lot more self-awareness now, which offers me the chance to adjust my plans. (Energy-level thinking and planning helps here, too.)
Brian went in to the office one day last week (he’s a permanent remote employee—even pre-pandemic—so that’s rare). Feeling physically decent-enough, I cleaned and tidied the house while he was gone.
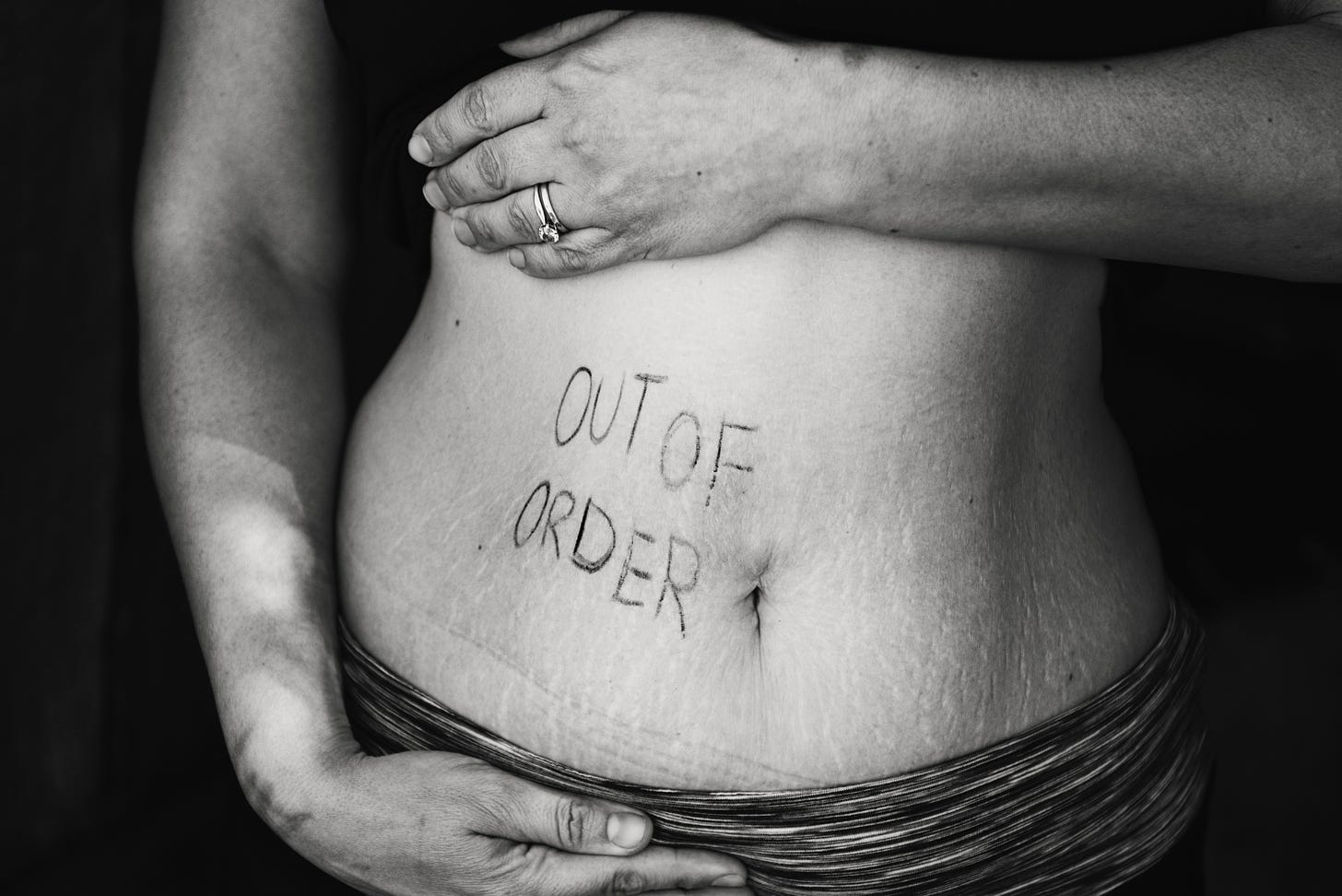
Inflammation is still high. Every muscle feels swollen. Every joint is stiff. As I type, I need breaks because my finger joints get stuck, and I have to wait for them to unlock. My brain can’t focus for longer than 5 minutes at a time. My nose tickles and itches, and I can’t stop rubbing it. I sniffle at random. My eyes itch. My feet hurt (connective tissue). My skin is red and bumpy, and sometimes feels like it’s on fire. I swing between heart palpitations, a heart rate so slow it feels like I’ll hit the floor, and tachycardia. And my gut has bursts of discomfort here and there. Which circle me back around to the focus part:
It’s so difficult to do anything when pain and discomfort rule the body and brain.
I really did a number on myself this time.
But I’m determined to get the word out.
Many healthcare professionals have no idea what Mast Cell Activation Disorder/Syndrome (MCAD/MCAS)1 even is.
Even in Seattle, I have to stick to my tight network of specialists for care and advice.
While in one of my worst flares before my immunologist-prescribed medications, I desperately searched for a doctor who could help. After an extensive search, I called a dozen or so offices that claimed MCAS specialization. But, after calling the first three, none of their office staff had heard of it.
“How do you spell that?”
Clearly, they didn’t “specialize” in it….
I received call-back variations of: “Hello. We are willing to look into your… condition. Dr. (X) said they’re happy to see you. Call us back at [phone number] to schedule. Thank you.”
I didn’t return those voicemails.
It makes me think of the practitioners in Florida. They tested and checked everything under the sun, except where I said the pain was. One even going as far as to take my uterus when it was Celiac Disease all along.
But I trusted them because they paid out the ass for higher education, so clearly they must be smarter than me, right? (Sarcasm)
But each one passed me off to another once they did everything they knew of to do, yet none of it got me closer to living a life.
I’d rather not be unfair. But, when you hear, “You need to lose weight” as the first line after you just told every single one of them that you can’t stand up for even 5 minutes without excruciating pain, you quickly realize that medical professionals are still flawed humans with bias and, sometimes, are straight-up ignorant.2
Money and education can’t (always) fix that.
Several practitioners later, and I finally got one answer I needed.
Almost 100 pounds (45.36 kg) melted off me within 9 months after cutting gluten post-Celiac Disease diagnosis.
Being fat wasn’t the problem. But maybe the inflammation from Celiac Disease was.3
An undiagnosed friend seems to share a few of my MCAS symptoms, and I'm worried about her. Mast cell disorders can worsen beyond repair (when anaphylactic levels are reached) if unmanaged, and in many cases become dangerous if it goes undiagnosed.4
As a fat person (meaning we’re regularly overlooked and disregarded within the medical community),5 it took an additional 6 years after my Celiac diagnosis to diagnose and begin managing MCAS. And I had to figure it out and bring it my doctors for testing.
But, according to a portion of the MCAS community, doctors struggling to figure out this affliction is common.
The Genetic and Rare Diseases Information Center6 summarized that:
Mast cell activation syndrome (MCAS) causes a person to have repeated severe allergy symptoms affecting several body systems. In MCAS, mast cells mistakenly release too many chemical agents, resulting in symptoms in the skin, gastrointestinal tract, heart, respiratory, and neurologic systems. Mast cells are present throughout most of our bodies and secrete different chemicals during allergic reactions. Symptoms include episodes of abdominal pain, cramping, diarrhea, flushing, itching, wheezing, coughing, lightheadedness and rapid pulse and low blood pressure. Symptoms can start at any age, but usually begin in adulthood. The cause of MCAS is unknown. Diagnosis is based on the symptoms, clinical exam, and specific laboratory testing. Other conditions may need to be excluded before MCAS can be diagnosed.
There are three known variants of Mast Cell, as Healthline breaks down:7
Primary MCAS occurs when a certain mutation, known as the KIT D816V mutation, is found and the mast cells display CD25, often with a confirmed case of mastocytosis. Mastocytosis8 occurs when the body produces too many mast cells.
Secondary MCAS occurs as an indirect result of another immunologic condition, IgE-mediated allergen (food or environmental allergy), or hypersensitivity to another trigger.
And Idiopathic MCAS. Idiopathic means that the cause of MCAS can’t be determined. Unlike primary MCAS, it’s not the result of a cloned cell. And unlike secondary MCAS, a doctor or healthcare professional can’t determine an underlying trigger for the MCAS.
I have Idiopathic MCAS—the one where it's cause is unknown.
I’ve struggled my whole life with the heat, sun, and numerous foods. These issues happened since early childhood. And they only seem to have gotten worse with age, pregnancies, surgeries and more.9
Basically, life made the condition(s) worse, as far as I can tell. (Then SciShow on YouTube threw a curveball with an exploration into autoimmune diseases, and how far more women have them.)
One day, not too long ago, my kids asked for pork buns from their favorite dumpling place nearby. One of them realized that would exclude me, but I said it was fine. “Well, there are advancements on the ‘Celiac pill,’10 so one day Mom could join us,” Brian chimed.
I joked, “Well, MCAS will still be a problem. But, at least that won’t kill me (unlike Celiac).”
As soon as I said it, something felt off. Later, I looked it up, and just like my gut hinted—and outside of the anaphylactic risk—it could.11
“People with SM [Systemic Mastocytosis] and MCAS are frequently reassured that they will live a normal life span,” wrote Lisa Klimas on MastAttack[dot]org.
She continues:
… [but] throw in a patient population as small as ours, and you’ve got a lot of uncertainty.
The effects of mast cell disease are highly individualized. There are several B and C findings, meaning that combinations of symptoms and manifestations are very variable.
And let’s not forget about the dangers of chronic inflammation—a major factor in mast cell disease— and its effects on the body.12
Cleveland Clinic writes:
With [long-term] inflammation, your body is on high alert all the time. This prolonged state of emergency can cause lasting damage to your heart, brain and other organs. For example, when inflammatory cells hang around too long in blood vessels, they promote the buildup of dangerous plaque.
With the added strain on the heart, lungs, brain, and body, in general, it’d be unwise to think one can go through life taking constant internal hits that not only affect the quality of life, but, potentially, one’s lifespan as well.
But Lisa Klimas also pointed out:
It’s okay to be scared. We all know people who have died from mast cell disease. It is scary to think that we could be next. It is scary to live under the looming threat of anaphylaxis. But the good news is that science is trying to catch up. More people are being diagnosed with mast cell disease, and science is getting better at identifying the ways that we are alike and different. There is every reason to think we will have comforting data in the future. We just have to get there.
Okay, why do I share all this?
Outside of caring, I want to spread the word on this still-considered rare but growing disorder.
I share because, with folks' prior Covid-19 infections, MCAS is on the rise. I could see it early on in how the MCAS community exploded online during the height of the pandemic with people getting newly diagnosed post-Covid infection. But the research shows a lot more than conjecture.13
PubMed wrote:
Mast cells (MCs) are activated by SARS-CoV-2. Although only recently recognized, MC activation syndrome (MCAS), usually due to acquired MC clonality, is a chronic multisystem disorder with inflammatory and allergic themes, and an estimated prevalence of 17%.
I want to get the word out as much as possible.
I won’t say my life is “ruined” or anything. But if we’d caught it sooner, life would be much easier—I can say with certainty. My hope is to bring information forward, so maybe you or someone you know who may suffer from at least two systems reactions as listed above, can catch MCAS before it gets to irreversible anaphylactic levels.
I hope you’ll send this to someone you care about. Maybe someone you know of who’s going through some mysterious issues that they’ve been unable to connect the dots on.
I learned about MCAS through a chronic illness podcast episode that I only found after discovering autism. And it took almost 3 years to get diagnosed and begin proper treatment.
Time is of the essence. I hope this can buy you or someone you know some more.
Be sure to check out the footnotes. But here are some additional resources:
If you’d prefer a video, here’s Cells | Normal role, allergies, anaphylaxis, MCAS & mastocytosis by Clevalab
8 Signs of Histamine Intolerance or MCAS, Functional Diagnostic Healing
The Many Co-Morbidities of MCAS, Mast Cells United
And as a PoTS sufferer as well: Do You Have Inflammatory PoTS (Postural Orthostatic Tachycardia Syndrome)?, PoTS Care
My best,
Sara
P.S. I predominantly write from my personal experience as an Autistic person with ADHD, chronic illness, Anxiety, and more. Each of these factors can influence my individual experience overall, as well as my experience of each condition.
What I share is not a substitute for medical advice.
Self-identification of Autism and ADHD (what many call “self-diagnosis”) is perfectly valid. If a personal Autistic experience I write about resonates deeply with you, consider these resources on Embrace Autism (starting with the Autism Quotient Test) as a first step. If professional assessment is important to you or your life has been impeded enough that you may need to qualify for Disability, you can print your results to bring to a diagnostician. (Having all those tests completed in advance saved me a lot of money!) Although there are many more diagnosticians available, here is a comprehensive list to get you started.
Lastly, some of my opinions may have changed since I first wrote the piece that lead you here.
Comment with any questions, and I’ll respond as soon as I can.
Help keep these posts coming by becoming a paid subscriber, buying my planner for professionals, buying me a “cup of coffee,” and even sharing and “Liking” this post helps, too.
I appreciate you whether you contribute a lot, a little, or even if you can’t right now. Thanks for being a subscriber, and thanks for reading.
Patient Questions: Is Mast Cell Disease autoimmune?, Mast Attack
More on Mast Cell Activation Syndrome, PoTS UK
Addressing weight bias in medicine, Harvard Health
Mast Cell Activation Syndrome: About the Disease, Genetic and Rare Diseases Information Center
The variations of Mast Cell Activation Syndrome (MCAS), Healthline
Mastocytosis, Cleveland Clinic
Symptoms of mast cell activation, Annals of Allergy, Asthma & Immunology
On prognosis and dying from mast cell disease, Mast Attack
Why You Should Pay Attention to Chronic Inflammation, Cleveland Clinic





